Bacteriology:
Based on the relative complexity of their cells, all living organisms are broadly classified as either prokaryotes or eukaryotes.
Bacteria are prokaryotes. The entire organism consists of a single cell with a simple internal structure. Unlike eukaryotic DNA, which is neatly packed into a cellular compartment called the nucleus, bacterial DNA floats free, in a twisted thread-like mass called the nucleoid.
Bacterial cells also contain separate, circular pieces of DNA called plasmids. Bacteria lack membrane-bound organelles, specialized cellular structures that are designed to execute a range of cellular functions from energy production to the transport of proteins. However, both bacterial and eukaryotic cells contain ribosomes. These spherical units are where proteins are assembled from individual amino acids, using the information encoded in a strand of messenger RNA
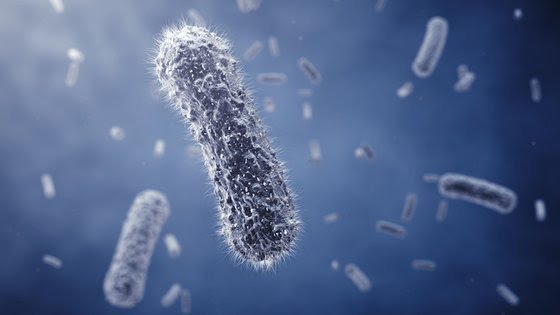
On the outside, bacterial cells are generally surrounded by two protective coverings: an outer cell wall and an inner cell membrane. However, certain bacteria, like the mycoplasmas do not have a cell wall at all. Some bacteria may even have a third, outermost, protective layer called the capsule. Lastly, bacterial surfaces can be covered by whip-like extensions: flagella or pili. According to the authors of “Mims Medical Microbiology, 5th Ed” (Saunders, 2013), long flagella aid in motility while short pili help bacteria to attach to host surfaces.
Classification
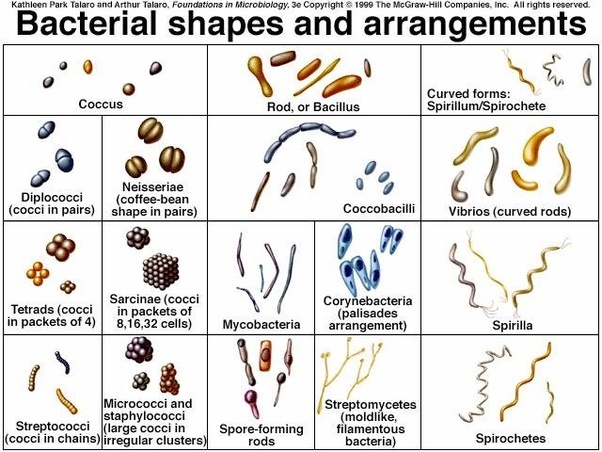
A few different criteria are used to classify bacteria. They can be distinguished by the nature of their cell walls, by their shape, or by differences in their genetic makeup.
The Gram stain is a test used to identify bacteria by the composition of their cell walls. It is named for Hans Christian Gram, who developed the technique in 1884. Bacteria are first stained with a purple dye called crystal violet, which specifically binds to peptidoglycan, a complex structure of amino acids and sugars found in the cell wall. This is followed by a series of steps that ultimately remove any unbound or loosely bound crystal violet.
Then the cells are stained with a second red-colored dye called safranin. Gram-positive bacteria stain purple because their cell walls are rich in peptidoglycan. On the other hand, Gram-negative bacteria whose cells walls have two layers take on a red coloring. The outer layer of lipids does not bind strongly to crystal violet and the dye is easily washed away during the staining process. For example, Streptococcus pneumoniae, which causes pneumonia, is a Gram-positive bacterium, while Escherichia coli (E.coli) and Vibrio cholerae, which causes cholera, are Gram-negative bacteria.
There are three basic bacterial shapes, according to “Mims Medical Microbiology.” Round bacteria are referred to as cocci (singular: coccus); cylindrical, capsule-shaped bacteria as bacilli (singular: bacillus); and spiral bacteria are aptly called spirilla (singular: spirillum). Cocci can also associate with one another in different configurations: combinations of two or diplococcus; a linear chain or streptococcus; and a cluster or staphylococcus. The shapes and configurations of bacteria are often reflected in their names. For example, the milk-curdling Lactobacillus acidophilus are bacilli, and pneumonia-causing Streptococcus pneumoniae are a chain of cocci.
The classification criteria mentioned thus far are based on physiological properties and morphology. However, classification of bacteria based on their evolutionary relationships to one another, that is to say, drawing a sort of family tree of all bacterial species, is a relatively new development. This type of phylogenetic classification became possible with the advent of nucleotide sequencing technology (the ability to read the order of nucleotides in DNA or RNA). Since ribosomes are present in all living organisms, one can look at similarities and differences in the RNA sequences that encode certain ribosomal proteins and determine the degree of relatedness of different organisms.
In his essay, “How We Do, Don’t and Should Look at Bacteria and Bacteriology,” included in “The Prokaryotes, 3rd Ed, Vol. 1” (Springer, 2006) Carl Woese notes that sequencing ribosomal RNA (rRNA) allowed for the development of a “clear concept of a bacterium” by establishing phylogenetic relationships between bacterial species. Using early sequencing technology developed by Frederick Sanger in the mid-1960s, Woese began to characterize bacterial rRNA and discovered a second group of prokaryotic organisms called archaea. Until then, the only known members of this group, the methanogens, had been mistakenly identified as bacteria. In their 1977 paper published in PNAS, authors Woese and George Fox state that methanogens bore “no phylogenetic resemblance” to bacteria.

Photomicrograph of Streptococcus pyogenes bacteria. Original Image
Credit: CDC
Reproduction
Most bacteria multiply by a process called binary fission. A single bacterial cell, the “parent,” makes a copy of its DNA and grows large in size by doubling its cellular content. The doubled contents are pushed out to either end of the cell. Then a small fissure emerges at the center of the parent, eventually splitting it into two identical “daughter” cells. Some bacterial species such as cyanobacteria and firmicutes reproduce via budding. During budding, the daughter cell grows as an offshoot of the parent. It starts off as a small nub, grows until it is the same size as its parent, and splits off
The DNA found in parents and offspring after binary fission or budding is exactly the same. Therefore bacterial cells try to introduce some variation into their genetic material by integrating additional DNA into their genome. This is known as horizontal gene transfer, and the resulting genetic variation ensures that bacteria can adapt and survive as their environment changes. There are three ways by which this occurs: transformation, transduction and conjugation.
During transformation, bacterial cells integrate short fragments of DNA from their surrounding environment. According to the authors of “Mims Medical Microbiology,” these fragments may be released by nearby bacteria that have ruptured. On the other hand, transduction occurs when bacteria are infected by special viruses known as bacteriophages that can carry bacterial DNA.
Conjugation requires physical contact between two bacteria. Genetic material, usually a duplicated plasmid, will transfer from a donor to a recipient. This plasmid copy travels out through a physical extension called the pilus and enters the recipient bacterial cell. Donor bacteria contain a sequence of DNA called the F-factor that enables pilus formation. Conjugation can aid in the spread of antibiotic resistance genes.
Bacteria in human health and disease
Bacteria can be beneficial as well as detrimental to human health. Commensal bacteria, which share space and resources within our bodies, tend to be helpful. In a 2012 article in the journal Nature, titled “Learning About Who We Are,” David A. Relman, a microbiologist at Stanford University, states that there are about 10 times more microbial cells than human cells in the human body. The highest numbers of microbial species are found in the gut.
The human gut is a comfortable setting for bacteria, with plenty of nutrients available for their sustenance. In a 2014 review article, “Analyzing the Human Microbiome: A ‘How To’ Guide for Physicians,” in the American Journal of Gastroenterology, the authors mention that gut bacteria and other microorganisms aid in digestion, stave off colonization by harmful pathogens, and help in the development of the immune system. Moreover, the disruption of gut bacteria has been linked to certain disease conditions. For instance, patients with Crohn’s disease have increased antibodies against their gut bacteria and their T-cells are quite aggressive toward bacterial antigens, according to the authors of “Gut Flora in Health and Disease,” published in The Lancet journal in 2003.
Other bacteria can cause infections. For example, Streptococcus pneumoniae causes pneumonia. Several bacteria ranging from group A Streptococcus, Clostridium, Escherichia coli and Staphylococcus aureus can cause a rare but severe soft tissue infection called necrotizing fasciitis sometimes called “flesh-eating bacteria.” According to the Centers for Disease Control, this infection affects the tissues surrounding muscles, nerves, fat, and blood vessels but it can be treated, especially when caught early
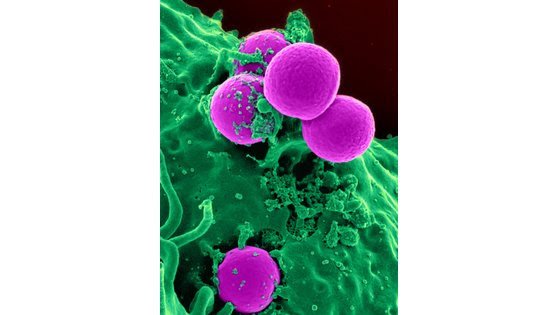
Antibiotic-resistant strains of Staphlyococcus aureus bacteria (purple) have become the most common cause of skin infections seen in hospital emergency departments. Original Image
Credit: NIH’s National Institute of Allergy and Infectious Diseases.
Antibiotic resistance
Antibiotics are typically used to treat bacterial infections. However in recent years, the improper or unnecessary use of antibiotics has promoted the spread of several strains of antibiotic-resistant bacteria.
Antibiotic resistance is a phenomenon where infectious bacteria are no longer susceptible to previously effective antibiotics. According to the CDC, each year in the United States, at least 2 million people are infected with antibiotic resistant bacteria, leading to the death of at least 23,000 each year. “Pretty much any infection you can think of now has been identified as being associated with some level of resistance,” said Dr. Christopher Crnich, an infectious disease physician and hospital epidemiologist at the University of Wisconsin Hospitals and Madison Veterans Affairs Hospital. “There’s very few infections that we now treat where infections caused by resistant bacteria is not a clinical concern.”
One of the more notorious antibiotic resistant bacterial strains is methicillin-resistant Staphylococcus aureus (MRSA), which resists methicillin and other antibiotics used to treat Staphylococcus infections. It spreads primarily through skin contact. MRSA infections occur in health care settings such as hospitals and nursing homes, where it can lead to pneumonia or bloodstream infections. MRSA also spreads in the community, especially in situations where there is a lot of skin contact or the use of shared equipment; for example, among athletes, in tattoo parlors, or in day care facilities and schools. Community-acquired MRSA most often causes skin infections.
An important facet of combating antibiotic resistance is to be careful about their use. “It’s so important for us to use antibiotics intelligently,” Crnich told LiveScience. “You only want to use an antibiotic when you have a clear cut bacterial infection.”